Scientific Overview
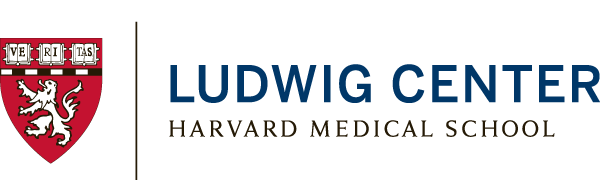
Despite advances in cancer therapeutics, most patients eventually relapse and succumb due to the development of resistance to therapies. The Ludwig Center at Harvard team has generated an overall strategy for addressing therapeutic resistance in order to overcome the challenges posed by the complexity, heterogeneity and plasticity of human tumors.
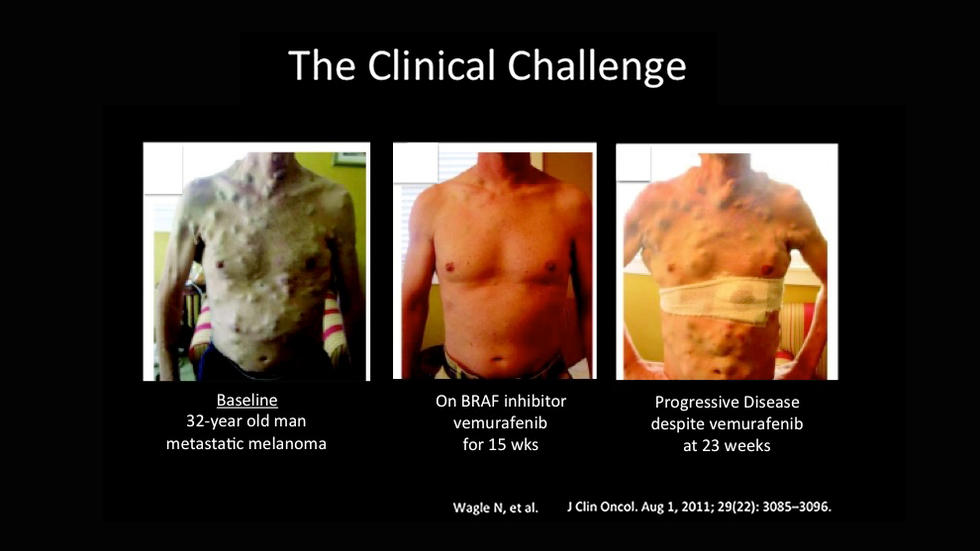
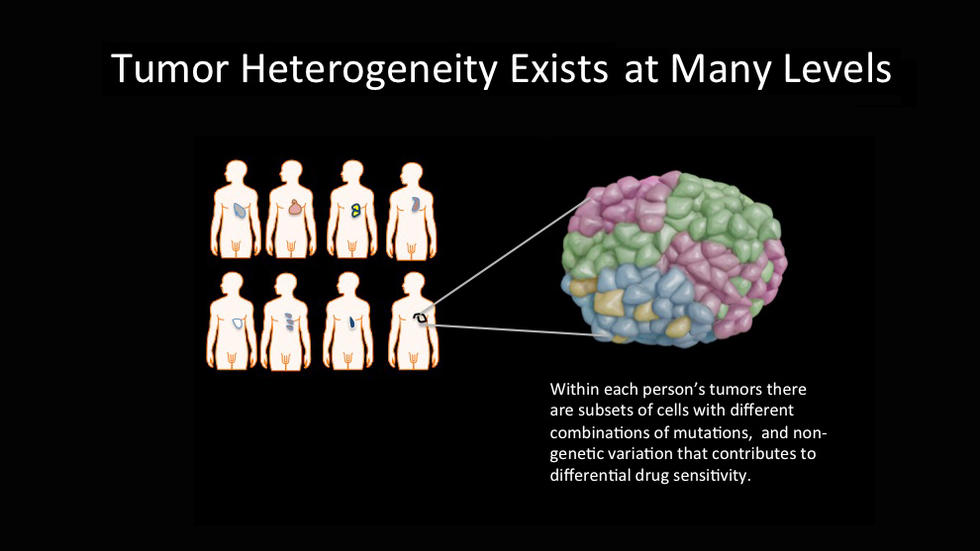
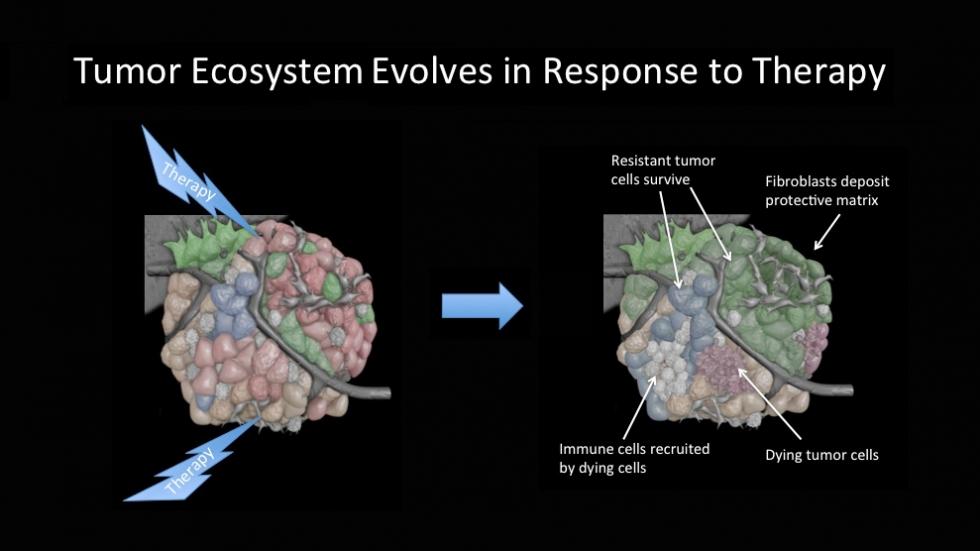
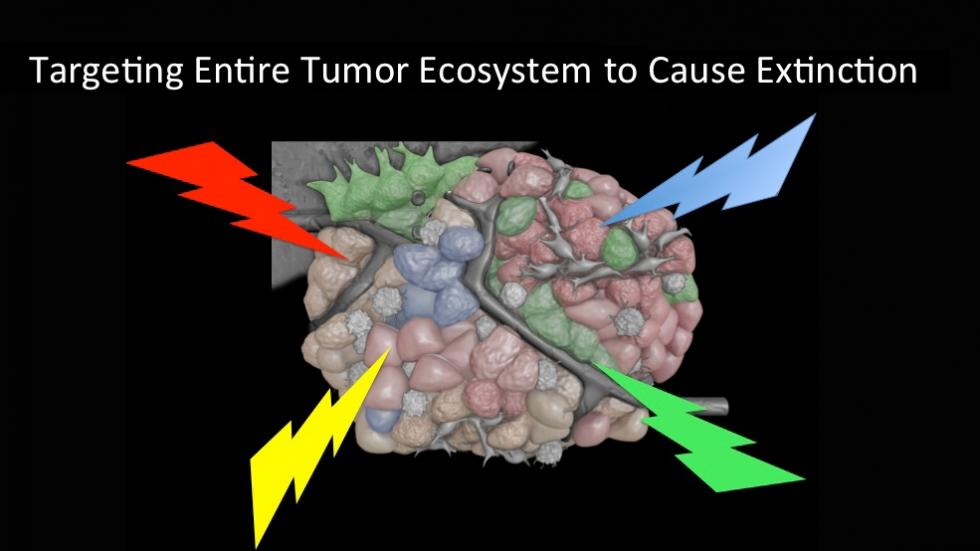
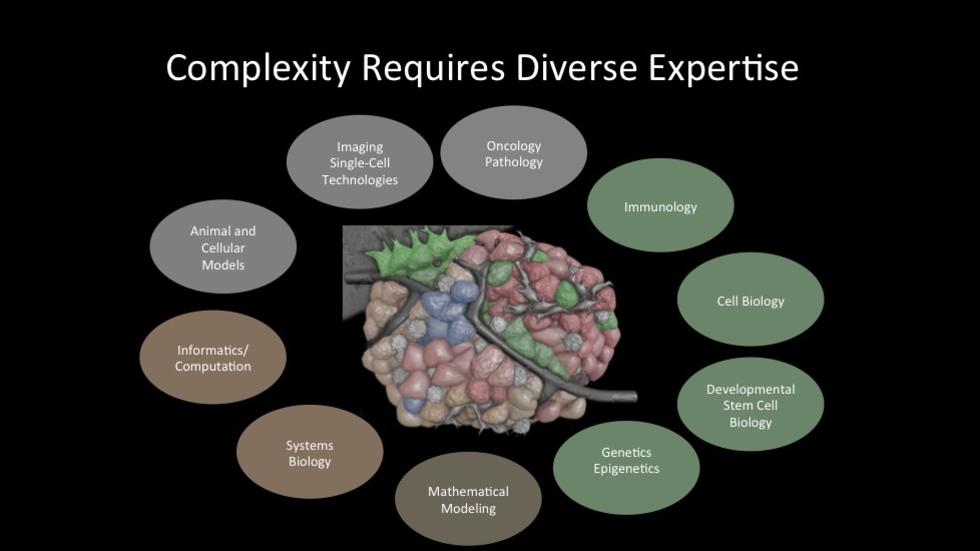
The resistance problem is complicated by tumor heterogeneity– this includes heterogeneity between tumors from different individuals, but even more significantly, within an individual tumor and between tumors at different sites in the same patient. The complexity and plasticity of the tumor and its microenvironment further exacerbates this problem, as therapeutic treatment can create new microenvironments that select for resistant subpopulations of tumor cells. Overall, the tumor ecosystem is highly robust due to the genetic and phenotypic plasticity of tumor cells and stromal cells and can adapt to multiple perturbations. However, based on known behaviors of other population ecosystems, we hypothesize that there is a limit to the number of perturbations that tumor cells can tolerate and that we can perturb a set of vulnerabilities to extinguish the ecosystem. Because the extraordinary complexity of the resistance problem presents challenges that no single laboratory can conquer in isolation, the Ludwig Center brings together a diverse group of scientists from across the Harvard community to work collaboratively to devise new strategies to overcome resistance. We focus on the underlying cellular programs, or "non-oncogene addictions" of tumor cells that are critical for the maintenance of tumor viability, while also integrating microenvironment factors, including those targeted by immunotherapy.